Contents
Effective teamworking and culture
Maternity Voices Partnerships and engagement
Foreword
In most cases pregnancy and birth are a positive and safe experience for women and their families. This is the outcome that everyone working in maternity services wants every time, for every woman. But when things go wrong, we need to understand what happened, and whether the outcome could have been different. The death or injury of a new baby or mother is devastating and something that everyone working in the health and care system has a responsibility to do all they can to prevent.
Last year, CQC’s briefing Getting safer faster: key areas for improvement in maternity services highlighted our continued concerns about the variation in quality and safety of maternity services across the country. Despite the greater national focus on maternity in recent years and the welcome improvements it has led to, the pace of progress has been too slow and action to ensure all women have access to safe, effective, and truly personalised maternity care has not been sufficiently prioritised to mitigate risk and help prevent future tragedies from occurring.
We were pleased to see that recommendations in the first Ockenden Report (December 2020) supported our view that improvements in the key areas of training and true engagement and involvement with individuals and groups who use maternity services through Maternity Voices Partnerships are required.
Following the publication of ‘Getting safer faster’ we launched a programme of risk-based, focused maternity safety inspections involving a more focused in-depth assessment of relational elements such as teamworking and culture, staff and patient experience.
Building on our previous calls for action, we also sought to further explore the barriers that prevent some services from providing consistently good, safe care and to better understand the disparities in outcomes that exist for women and babies from Black and minority ethnic groups.
This report presents the key themes from nine of those inspections alongside insight gathered from direct engagement with organisations representing women using maternity services and their families, including Five X More and local Maternity Voices Partnerships. While based on only a small sample of inspections, and therefore not representative of a national picture, the report captures the key issues that we found persisting in some services, and that we are concerned may be occurring to some extent in other maternity units.
We know that there are many maternity services that are providing excellent care, but we remain concerned that there has not been enough learning from good and outstanding services - or enough support for that learning from the wider system. Issues such as the quality of staff training; poor working relationships between obstetric and midwifery teams, and hospital and community-based midwifery teams; a lack of robust risk assessment; and a failure to engage with, learn from and listen to the needs of local women all continue to affect the safety of some hospital maternity services.
Although rare, serious complications and maternity deaths have a lasting impact on families and their loved ones. The devastation caused in such circumstances cannot be underestimated. It is essential that we have a system that is open, and that recognises, investigates, and learns when things go wrong, so that families get the truth, and safety continually improves.
We must also be honest about the inequalities that exist for some people. Women from Black and minority ethnic groups have poorer experiences of care and face additional risks. While maternal deaths are rare maternal mortality rates are significantly higher than for women from Black and minority ethnic groups than for women from White groups. Addressing inequalities in access and tailoring maternity services to best meet the needs of the local population is a critical area for action and something that good services are prioritising. We welcome the recent NHS pledges to improve equity for mothers and babies and race equality for staff.
The importance of good leadership, effective governance, a strong safety culture and a proactive approach to addressing health inequalities is not unique to maternity – they are fundamental components required across all services and typify the challenges we want to help tackle as part of our new strategy.
Safe, high-quality maternity care is not an ambitious or unrealistic goal. It should be the minimum expectation for women and babies – and is what staff working in maternity services across the country want to deliver. This report identifies areas for action with the aim of helping to accelerate the current pace of change and to support maternity services, along with their trust boards and stakeholders, to focus on the steps they can take now to ensure that women and babies get consistently good, safe care.
Impact of poor care
Tinuke’s story
From midway through my pregnancy there were signs of pre-eclampsia, including high blood pressure and protein in my urine. Pre-eclampsia is life threatening for both mother and baby, but it’s easily treatable. If you can spot it in time, it’s just an aspirin tablet that can vary your chances. However, I wasn’t diagnosed until a last-minute midwife appointment at the end of my pregnancy. By that time, I was so swollen that I was advised to go straight to the hospital by my midwife, which of course was really worrying to hear as a first-time mum.
At the hospital, I was told that I would need to be induced. My labour progressed really quickly, but the midwife refused to believe that I was actually in labour. I was left alone for hours without any pain relief. I remember at one point I was vomiting; I was literally bent over and there was fluid coming out everywhere – it was awful. By the time my waters finally broke and I was checked over I was eight centimetres dilated, so the window for being given any pain relief was gone.
By the time I was told I could push, I was so exhausted that I had to have an assisted delivery. It’s not how I wanted to bring my son into the world. The whole experience was extremely traumatic and could all have been avoided if I had been listened to.
Introduction
The risks to mothers and babies during pregnancy and in the postnatal period, and the opportunities to identify and manage them effectively, have been the subject of many inquiries and reviews. In 2015 the government set out an ambition to reduce the rates of stillbirths, neonatal deaths, maternal deaths and brain injuries in babies that occur during or soon after birth by 50% by 2030. This was then brought forward to 2025 in the Long Term Plan. To deliver on this ambition and the vision set out in Better Births, NHS England established the national Maternity Transformation Programme, of which CQC is an active member.
Our ratings data shows that the improvement in the safety of maternity services is too slow. In our report ‘The state of care in NHS acute hospitals 2014 to 2016’, published in April 2018, we raised our concerns that half of all maternity services were rated as requires improvement or inadequate for the key question ‘are maternity services safe?’. Our Getting Safer Faster briefing in March 2020 showed that this had improved slightly to 39%. Latest figures from July 2021 show that 41% of services are rated as inadequate or requires improvement (figure 1). It is important to note that this should be considered in the context of the more risk-based approach to inspection we have taken during the pandemic, which has meant that our inspections have been focused on those services where we have the biggest concerns.
Figure 1: Number and percentage of NHS maternity services by their rating for ‘safe’ from first rating (paler bars) to current rating (bold bars) (31 July 2021)
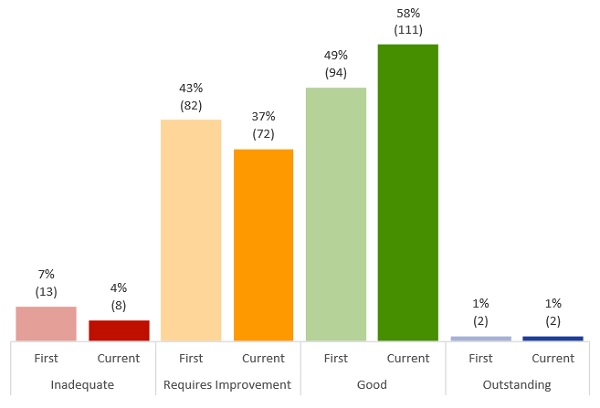
Source: CQC
Issues we have highlighted in our previous publications continue to cause concern. These include staff not having the right skills or knowledge; poor working relationships; poor risk assessments; and not learning from when things go wrong.
To explore these issues in more depth, we visited nine maternity services where we had concerns between March 2021 and June 2021. As part of these inspections, we also looked at how these services worked with their local Maternity Voices Partnerships to engage with women, and looked at what they were doing to address inequalities for women and babies from Black and minority ethnic groups and women from deprived groups.
It is important to note that this report reflects only what we found on our visits to a small number of services. It is not a national picture of all maternity services. However, we are concerned that many of the issues raised in our report may be occurring in other maternity services.
Challenges in maternity care for women from Black and minority ethnic groups
Women from Black and minority ethnic groups experience additional risks compared to White women that, without the right interventions, can lead to poor outcomes. For example, we know that:
- Black women are four times more likely to die in pregnancy and childbirth than White women. For Asian women it is two times more (read Saving Lives, Improving Mothers’ Care 2020).
- Mortality rates remain higher for Black or Black British babies and Asian or Asian British babies. While stillbirth rates for these groups have reduced over the period 2015 to 2017, neonatal mortality rates have increased over the same period (read Better Births Four Years On: A review of progress).
Further evidence of poorer maternity outcomes for Black and minority ethnic women can be seen in our analysis of Hospital Episode Statistics data on readmission rates per 1,000 deliveries from January 2018 to December 2020. This analysis shows a consistent trend of Black women having the highest rate of readmission to hospital during the six-week postpartum period, while White women consistently had the lowest rate. This includes any emergency or maternity related admission in that six-week period (figure 2).
Figure 2: Readmissions per 1,000 deliveries by ethnicity (January 2018 to December 2020)

Source: Hospital Episode Statistics
Our analysis, comparing readmission rates and their 95% confidence intervals, also suggests that Black women had a significantly higher rate of readmission in the postpartum period over the course of 2020 than all other women. There was a 30% difference between the readmission rate for Black women and rate for White women (93 readmissions per 1,000 deliveries for Black women compared to 68 readmissions per 1,000 deliveries for White women).
The additional risks faced by women from Black and minority ethnic groups have been exacerbated during the COVID-19 pandemic, highlighting the urgent need to improve equity in maternity. During the pandemic, the UK Obstetric Surveillance System (UKOSS) study found that more than half of pregnant women admitted to hospital with COVID-19 infection in pregnancy were from Black or other ethnic minority groups. Black women were also eight times more likely to be admitted to hospital with COVID-19 during pregnancy than White women, while Asian women were four times more likely.
In June 2020, the Chief Midwifery Officer, wrote to all NHS midwifery services highlighting the impact of COVID-19 and the additional risks faced by women and babies from Black and minority ethnic communities. The letter called on services to take four specific actions to minimise this additional risk.
As part of our inspections, we looked at how services were addressing these actions. We have also worked with Five X More and National Maternity Voices to better understand the issues faced by women from Black and minority ethnic groups, and help develop our approach to equity and engagement in our focused inspection programme.
It is important to note that when writing about ethnicity in this report we use the term women from Black and minority ethnic groups. This is the preferred term of CQC’s Race Equality Network when we are not able to refer to specific groups. In terms of census ethnicity categories, we intend this term to include women from the following groups:
- Black, African, Caribbean or Black British
- Asian or Asian British
- mixed or or multiple ethnic groups, or
- other ethnic groups
What we did
During 2019–20, we developed and piloted a programme of focused inspections to look specifically at the safety of maternity services. Building on the learning from these pilot inspections, between March 2021 and June 2021 we visited nine maternity services where we had concerns about the safety of the service and, alongside our focused inspection, we explored specific questions around teamwork, culture, equity and engagement. At the time of our visits, the country was emerging from the third COVID-19 lockdown and the NHS was starting to recover from the winter peak in cases. Like all services, this created challenges for maternity care.
Our activity included looking at the actions that services are taking in response to the letter from the Chief Midwifery Officer to ensure they are providing equitable care for women from Black and minority ethnic groups during pregnancy, such as provision of continuity of carer and how they are addressing additional risks from COVID-19.
As part of the visits, we also reviewed a small sample of maternity notes at some of the sites visited to check whether information around vitamin D, ethnicity and a number of risk factors was being recorded. Following inspection, inspectors were interviewed about their observations.
It is important to note that these inspections were not intended to cover every aspect of the current, larger, maternity core service inspection framework. However, we will use the findings from these focused inspections to support the development of our new operating model, in line with the themes of our new strategy.
In addition to our inspections, we interviewed 11 Maternity Voices Partnership (MVP) chairs – eight from the areas where we carried out our visits, and three from different areas. MVPs are an NHS working group made up of women and their families, commissioners and providers who work together to review and contribute to the development of local maternity care. Many MVPs are still in early stages of being established. We asked about their experience of working with maternity services to engage with their local population. This includes ensuring the voices of women using services are being heard. Themes emerging from these interviews were then explored in further detail through two engagement sessions with Five X More and National Maternity Voices.
Effective teamworking and culture
Key points
- In some services we found a lack of consistent and clear leadership, management, governance and assurance processes. This included a lack of oversight of services and problems in them.
- The culture of services we inspected varied, with evidence of poor working relationships between obstetric and midwifery teams, and hospital and community-based midwifery teams in some services.
- Poor teamworking, was also characterised by staff feeling unsupported or not feeling confident to seek support from senior colleagues or being afraid to challenge decision-making.
- While we saw some evidence of multidisciplinary team training, there were concerns that not all staff were engaged with training. The quality of training and support for staff to maintain and develop their individual capabilities and core competencies also varied between the trusts we looked at.
As we reported in Getting Safer Faster, successful services have good team working and an effective, collaborative leadership team. National maternity reports, including the first Ockenden review, Each Baby Counts Final progress report 2020, and the Morecambe Bay Investigation Report, have focused on why good clinical leadership is fundamental to successful maternity services.
Good leadership is crucial as it creates a team culture of inclusivity and openness with effective communication, escalation and clear routes of accountability. This is necessary for good clinical care and also helps to also drive a culture of safety and improvement.
This section explores the impact of leadership, teamwork and culture in maternity services.
Leadership and culture
The article ‘Understanding the dynamics of organisational culture change’, highlights that, in maternity services, the leadership team is strongest when the service level manager, midwifery and obstetric leaders are all in place and work well together to provide care that meets the needs of all women using the service.
The first Ockenden review set out initial findings from the independent review of the maternity services at the Shrewsbury and Telford hospital NHS Trust. This highlighted the importance of strengthening leadership and oversight for maternity, addressing toxic workplace cultures and fostering more collaborative approaches in maternity services.
In the services we inspected, we were concerned about the lack of consistent leadership and management teams, as well as weak links between parts of some maternity services. For example, in one service there was uncertainty about how a new standalone midwifery unit would integrate into the service as it wasn’t clear how it would be staffed. At another service, staff were not clear about arrangements for transferring women between units in the same trust.
We found that in some of the services we visited either the service level manager, midwifery leader or obstetrics leader was not in post, or that one of these positions was held by an interim postholder (most often the midwifery lead). The article ‘Understanding the dynamics of organisational culture change’ highlights that having a stable leadership team is known to improve organisations’ focus on patient safety. Despite improvements in midwifery leadership skills, there needs to be a more collaborative approach to developing leadership skills for maternity service leads. This includes developing formal leadership development programmes for maternity teams.
In a number of the services we looked at there was a lack of a common purpose and a sense of a maternity ‘team’. We heard that this could lead to a disconnect between midwives who worked in the community and those that worked in acute settings. For example, some community midwives told us that they felt their concerns about the complex needs of some of the women they looked after were not acted on. In some cases, these midwives had stopped reporting concerns as a result.
One provider had carried out work to review and strengthen the governance and assurance processes from maternity service level to board. Information about incidents was presented to staff in a weekly report. This information was then collated on a monthly basis for review by the service level leadership team, which included the Board Safety Champion. In turn, this formed the basis of the report to the trust quality committee. While this change was new, it was anticipated that staff would feel more empowered to report incidents because they would be able to see how the information would be used for learning and to make safety improvements.
Learning and improvement
In the article ‘Seven features of safety in maternity units’ it highlights that when staff feel able to speak up without fear of retaliation or embarrassment, it can lessen the development of harmful blame cultures and help to foster a culture of openness. In turn, this can help to improve the safety of the service. The article ‘Trends in healthcare incident reporting and relationship to safety and quality data in acute hospitals’ shows that services that encourage incident reporting can facilitate system learning. This leads to better standards of care and improved responsiveness to problems.
The culture of services we looked at in our review varied. At one trust, where the maternity service was split across three sites, we found cultures were very different between the locations. One site reported that staff felt respected, supported and valued, but another site reported the opposite. Despite having a single governance structure, there were no formal arrangements for staff to spend time across the sites. This could result in missed opportunities for learning.
We heard many examples of poor incident reporting across the services we visited. We found that in most services staff didn’t always recognise what constituted an incident or how to grade the incident correctly. We also heard about the pressures faced by staff with the practicalities of incident reporting. In one service, a midwife told us that they did not have time to report incidents due to the amount of activity in their work area.
More worryingly we found evidence at one service where some maternal deaths had not been reported via NRLS or investigated as serious incidents. At another service, some staff made allegations of cover-ups when things went wrong and that incidents were often not reported.
Despite these issues around incident reporting, most services we visited had processes in place to learn from incidents, though the extent to which these were successful varied. Examples of these processes included: identifying and categorising incidents, monitoring incidents using dashboards, ensuring appropriate communication and escalation of incidents.
Trusts with a learning culture tended to show more thorough learning from incidents, which translated into creating improvements. We saw evidence of this improvement during our inspections, with one service introducing formal cardiotocograph trace (CTG) training and support following incidents.
Services used a variety of methods to share learning. This included face-to-face events, such as open meetings, huddles and debriefs, as well as written newsletters, local intranet and posters.
In services that did not have a clear culture of learning, we found that action may not have been taken. For example, in one service, we heard that issues with language barriers and access to interpreters had been known about for many years, but the service had only just started to make changes following an external review.
In another service we witnessed a disconnect between the senior leadership team’s perceptions of incident management to the reality of the actions being taken on the frontline. For example, while managers told us that a short briefing was circulated to staff during daily handovers, in reality this was not taking place effectively.
Some maternity services told us that they used external reviews, for example by the Healthcare Safety Investigation Branch, as a way of receiving feedback and learning from incidents. We heard how the investigation reports were used by some services to identify themes, create action plans, develop new training and issue guidance to staff. In one service, the HSIB report highlighted concerns about the interpretation of CTGs. Following this review, the service implemented a new training programme that included a test to ensure that staff were competent to interpret CTGs in clinical practice.
While it is positive that services are seeking external support, in some cases services in our review appeared to rely too heavily on this process, for example delaying responding to or learning from incidents internally until after external review.
To further the learning process, some services told us about the progress they had made with quality improvement (QI). This is a structured approach, using set methods and tools, that seeks to continuously improve quality of care and outcomes for patients. One service told us that they had employed a dedicated QI midwife to lead and progress several projects and ensure that QI training was mandatory for all new midwives. Another service had created a maternity improvement group.
Support and teamwork
The culture of a service can have an impact on staff support and teamwork, with staff feeling less supported in hospitals that have a blame culture and/or cultural issues around staff bullying. For example, in one service we visited we saw evidence of a poor culture when a nurse mistook an inspector, who was dressed in scrubs, for a member of staff and shouted at them to answer the phone.
In the same service, multiple people reported being hesitant about challenging poor practice or decision-making due to fears around losing their jobs. In addition, different staff groups were accusing one another of bullying and this had led to a very hostile working environment with divisions between teams.
The NHS Improvement report on Shrewsbury and Telford’s handling of a review of its maternity services identified that poor cultures can foster poor relationships between staff members and result in a fear to challenge. The Each Baby Counts final report also highlighted that siloed working as a result of these environments can have a hugely detrimental impact on a woman’s care, particularly if there are concerns that need to be escalated to more senior members of both midwifery and medical teams.
While staff in some services felt comfortable seeking advice and support from senior colleagues, this was not the case for staff in other services. For example, staff in one service told us that they did not feel confident in knowing when to call a consultant in from home.” Some community midwives also told us that they did not feel able to raise concerns about the complexity of some women who had been booked for home delivery. Not being clear on when to involve consultants or lacking the confidence to liaise with colleagues to escalate concerns and seek support when required puts the safety of women and their babies at risk.
We welcome new guidance from the Royal College of Gynaecologists (RCOG) that outlines recommended standards to define when consultants need to be involved in discussions about patient care. This includes a trigger list of situations where consultants are expected to attend to make it easier for midwives to escalate concerns.
How well supported staff we met during our review felt was also influenced by staffing levels. Having fewer staff due to sickness, vacancies or strain from COVID-19 meant that people were less able to support one another.
This is supported by a 2019 article in the British Medical Journal, which raised the issue of problems with stress and burnout within maternity services, and the impact on the maternity workforce. It is also supported by The UK WHELM study, which highlighted that low levels of management support, professional recognition and opportunities for development contributed to burnout, depression, anxiety and stress.
Through our visits, we found that one service had tried to improve this situation by agreeing with their finance department that they could pre-empt a vacancy and hire new staff. As a result, this service did not have any vacancies. This stability had fostered good relationships in the department, and staff felt supported.
Despite his example of positive action, staffing has remained a challenge for others. For example, we heard that where services had interim and new leadership positions, staff felt less supported.
How services responded to incidents also affected how supported staff felt. For example, in one service senior staff had taken responsibility for incidents, while in another they had documented clear action points. As a result, staff felt better supported. We also heard of support being provided through ‘hot debriefs’ immediately after an incident and/or a meeting at a later date.
We also heard good examples of occupational health and specialist counselling being offered to staff following incidents. In one service, we heard about restorative sessions led by a representative from the professional midwife advocate. Feedback following incidents was reported to improve support throughout the incident process, and in some services had led to changes in training or the delivery of a service.
However, one service we visited reported that they found it challenging getting all staff together after an incident. While initial support was good, improvements were needed for longer term support.
The visibility of the senior leadership team was another theme that emerged from our review of maternity services. We found several services where the senior leadership team lacked visibility and staff relied on one another for support.
However, there were positive examples of engagement through staff surveys, listening events and walkarounds which contributed to staff feeling supported and safe. Across a number of services, we heard of measures including ‘wobble rooms’, a timeout pod and a wellbeing lounge.
Team training
The first Ockenden review of maternity services at Shrewsbury and Telford Hospital highlighted that ‘staff who work together must train together’. This has been supported by other clinical articles, published in the BJOG: an international journal of obstetrics and gynaecology and the British Medical Journal, that show evidence that multidisciplinary training in maternity can improve patient outcomes for both mothers and their babies.
In most of the services, we found evidence of regular multi-professional training but the impact of this training was not always consistent or evaluated.
In one service we visited, training involved both the medical and midwifery teams, and was centred around the themes emerging from incidents. This included the management of massive obstetric haemorrhage and shoulder dystocia. As a result of this training, the ROTEM machine (a machine used to analyse blood during massive obstetric haemorrhages) was used less as haemorrhages were better managed, and there were fewer admissions to the neonatal unit due to fractures from managing shoulder dystocia. The same service had also implemented ‘trolley dashes’. This involved educational staff visiting staff in different areas with a trolley full of equipment and doing quick learning sessions on topics such as postpartum haemorrhage and cord prolapse.
In another service we heard about a practice development manager who introduced unannounced ‘skills and drills’ sessions. These are short training sessions that are based on real themes from incidents used to improve practical skills and train for specific scenarios. For example, one of these sessions was based on the real-life incident of a woman giving birth to twins in the toilet. Other services reported using simulation suites and formal training programmes, such as trauma and risk management training.
While we saw some good examples of multidisciplinary learning, at other services some staff members, including consultants and anaesthetists, were not always attending multidisciplinary training. In addition, we found that skills and drills training was lacking in a few of the hospitals. As a result, we were concerned that staff did not have the required skills and knowledge to perform certain tasks. For example in two of the services we visited, we found that staff were not trained for the event of an emergency evacuation from the birthing pool. This could have potentially severe consequences on the management of emergencies.
The COVID-19 pandemic had a significant impact on the provision of training. To address this, the services we visited had mostly switched to delivering training virtually, with a hope to return to face-to-face training as the pandemic eased. One service reported that some of their training had been paused during the pandemic as staff were required to provide patient care and could not be released to attend training.
As well as providing multidisciplinary training, services must make sure that staff are supported to develop and maintain individual core competencies, and to work effectively as a team at all times. We are concerned that this is not happening. For example, at one service we heard that a lack of familiarity or ease with using instrumental delivery methods was a possible cause for Caesarean sections being performed at full cervical dilatation. Leaders of maternity services must tailor the training requirements for individuals to ensure that they are ‘fit for purpose’.
Equity in maternity services
Key points
- The majority of services we visited had carried out some work to implement the four actions from the Chief Midwifery Officer to support maternity equity for women from Black and minority ethnic communities. However, we were concerned that in many cases the actions had been interpreted quite narrowly.
- While maternity services should discuss the importance of vitamin D during pregnancy, recording of discussions about vitamin D was often inconsistent or absent in the services we visited. This creates the risk that vitamin D is not being discussed and/or offered to women who need it.
- The pandemic has meant that nearly half the services we visited had paused their continuity of carer teams. However, it was positive that where teams were in place, we saw a focus on women with higher risks.
- Engagement by both services and Maternity Voices Partnerships was often generic rather than tailored to better target different groups within their local population, such as women from Black and minority ethnic groups.
As part of our inspections, we looked at the arrangements services have put in place to address the four actions of the Chief Midwifery Officer to support Black and minority ethnic women and women living in deprived areas during the pandemic.
While we found evidence of services addressing some of these actions, we were concerned that in many cases the actions had been interpreted quite narrowly rather than considering what further actions were needed to make services truly equitable and safer for all women, as well as ensuring that all women felt informed and supported. We heard limited evidence about additional work that services were doing to support equitable access outside of the four actions.
Two positive exceptions were where services had created specific roles to promote equity. One service had created a midwifery role to work on the policies and pathways to deliver care to women from Black and minority ethnic groups, and another had introduced an equality and inclusion role to assess the training needs of staff. However, in both cases, it was too early to tell whether these roles were having a positive effect on equity.
This section explores in more detail what we found in relation to the four actions, continuity of care and engagement with women from these communities.
Action 1: Increasing support of at-risk pregnant women
At four trusts where we looked at this directly, we were told that in line with the first action from the Chief Midwifery Officer they had reduced the threshold for women from Black and minority ethnic groups to come in for assessment at the day assessment unit or labour ward for medical review.
In some services, we heard that staff were aware of the higher risks faced by women from Black and minority ethnic groups. Steps taken to increase awareness included adding relevant risks on to triage forms, holding monthly multidisciplinary meetings to discuss women at high risk, and reminding midwives and clinicians of the increased risks for these women.
Action 2: Reaching out and reassuring pregnant women from Black and minority ethnic groups with tailored communications
We looked directly at this issue in seven of the maternity services we visited. How well maternity services had used tailored communications to reach pregnant women from Black and minority ethnic groups varied.
In a few trusts we heard that they had worked collaboratively with their Maternity Voices Partnerships (MVPs) to co-produce videos to share messages around accessing care and the additional risks for certain groups. One MVP chair described how they worked with a mother with a young baby, who is a GP and a Black woman, to create a video talking about the risks and misconceptions for Black women during pregnancy, birth and postpartum and the importance of taking Vitamin D during pregnancy. This video was then shared via social media.
Another service had worked in partnership with the local MVP to share information around risks for women from Black and minority ethnic groups using a mobile application.
We heard of services using other methods of contact to reach out to women of Black and minority ethnic groups. For example, one service had used the information they held on women’s ethnicity to write to all women from Black and minority ethnic groups to advise them on good health and risk reduction during pregnancy throughout the pandemic.
However, heard of services using other methods of contact to reach out to women of Black and minority ethnic groups. For example, one service had used the information they held on women’s ethnicity to write to all women from Black and minority ethnic groups to advise them on good health and risk reduction during pregnancy throughout the pandemic.
At another service we heard an allegation that there was discriminatory behaviour from staff towards women who did not speak English. We were given an example of a midwife shouting at a woman because she could not understand English. Senior leadership were aware of concerns around how staff treated the women who used the service and said they had begun to challenge these behaviours. An external review had previously identified risks with women who have difficulty reading or speaking English being unable to access interpreters. In response, the service had installed phones in rooms to improve access to interpreters.
While it is positive that some services were taking steps to try to reach out to and involve women from Black and minority ethnic groups, there were some concerns about how this was being done. For example, reliance on digital technology, such as sharing information via Facebook, risked excluding women who did not have access to or were not comfortable using the internet.
Through our engagement with Five X More and National Maternity Voices we also heard concerns that sharing information about risks, without empowering women to understand what these risks mean and any steps they can take to minimise them, could be scary for women and lead them to disengage or limit contact with maternity services.
Action 3: Ensuring hospitals discuss vitamins, supplements, and nutrition in pregnancy with all women
It is well known that due to low sunshine levels, people living in the Northern Hemisphere may not get enough vitamin D, and women from Black and minority ethnic groups who have melanin pigmented (darker) skin, or who cover their skin when outside, may be particularly at risk. As a result, the Royal College of Obstetricians and Gynaecologists advises that all pregnant women consider taking 10 micrograms of vitamin D a day to keep their bones and muscles healthy. The National Institute for Health and Care Excellence (NICE) guideline ‘Vitamin D: supplement use in specific population groups’ also recommends that health professionals discuss and record this with all pregnant women.
At some of the services we visited, we found that discussions about vitamin D were not being consistently documented. This creates the risk that vitamin D is not being discussed and/or offered to women who need it.
Only three out of the 10 sites we inspected were recording vitamin D in all the notes reviewed, and at five of the sites vitamin D was not documented in any of the notes reviewed.
Action 4: Recording of ethnicity and other risk factors for all women
Ethnicity was recorded in the majority of women’s maternity case notes at most of sites we visited. However, recording of other risk factors was more variable. For example, across the nine sites where we reviewed a small sample of maternity notes, only three consistently recorded age. A similar picture was seen when recording body mass index (BMI) and postcode. We were unable to confirm whether this was because services were only recording this information where there were concerns relating to age, BMI or social deprivation.
While it is positive to see that the majority of services we visited were recording information about women’s ethnicity, it was not always clear whether services were using this information, for example to review outcomes for women from Black and minority ethnic groups, using this information effectively, to learn from incidents or to personalise care. As a result, inequality may not be recognised as a safety issue. Important differences in experiences and outcomes for Black women compared to women from Asian or mixed heritage groups – or White women – can be missed.
Similarly, where services were not consistently recording risk factors such as a person’s BMI, this meant they would not be able to use this information to review and make changes to the care and support offered.
Through our work with Five X More we also heard concerns about using the equality data collected to stimulate change. We heard that while the increased risk of poor outcomes for Black and minority ethnic women is well established nationally, there is currently no national target to reduce these inequalities.
Our work with Five X More has confirmed to us the importance of collecting and reviewing data to stimulate change, and ensure that opportunities for learning are not missed. This includes measuring the impact of such changes.
Continuity of carer
The 2016 Cochrane Review highlighted that women who receive midwife-led continuity of carer are less likely to experience pre-term births or lose their baby in pregnancy, or in the first month following birth.
The continuity of carer scheme was set up to provide consistent, coordinated care throughout women’s pregnancies. The NHS Long Term plan set out a target that by March 2021, most women would receive continuity of the person caring for them during pregnancy, during birth and postnatally. It also set out the target that for women from Black and minority ethnic groups, and women from deprived groups, 75% should receive continuity of care by 2024, as it has been linked to significant improvements in clinical outcomes for these women.
At the time of our inspections, just over half of the services we inspected had active continuity of carer teams providing support to small numbers of women in their community they had identified as being at higher risk. Where services did not have these teams in place, we heard that they had either been put on hold or disbanded, primarily due to staffing issues in the pandemic.
None of the continuity of carer teams had an explicit focus on supporting women from Black and minority ethnic groups. However, one service had plans to identify Indian women who would be looked after by the continuity of carer teams. Another team had focused their resource on a geographical area with a relatively high proportion of women from Black and minority ethnic groups. Other continuity of carer teams were focused on deprived areas, women with diabetes, women with previous maternity loss and other vulnerable groups.
Safeguarding
An MBRRACE rapid review, published in May 2020, highlighted the safeguarding risks to women from domestic violence, mental health and systemic biases. These interrelated risks can prevent women with complex and multiple problems receiving the care they need, and impact on the care of Black and minority ethnic women. While these risks are not new, evidence from statutory and voluntary agencies suggests that the risks increased during lockdown. For example, Refuge reported a 60% increase in calls and online requests following the start of the first lockdown in March 2020.
We looked at what action services were taking in relation to safeguarding in eight of the maternity services we visited. We heard about a range of specialist clinics and specialist midwife roles in place to support women around safeguarding. This included bereavement clinics, female genital mutilation (FGM) clinics (previously traumatic experience clinics), as well as midwives specialising in teenage pregnancy, perinatal mental health, vulnerable women and FGM.
We heard that during the pandemic, two services had noted an increase in domestic violence cases. Another service was putting together a business case for a midwife role specialising in domestic violence. However, at one service we found that they were not recording whether domestic violence was assessed during all appointments, which was a risk. This service had picked up on the need to educate staff around domestic violence and were running pop-up sessions to educate staff around the risks and indications for safeguarding.
Targeted engagement
We found limited evidence that the maternity services we visited were targeting engagement towards women from Black and minority ethnic groups and women living in deprived areas. Only three out of seven trusts described specific pieces of engagement work they had carried out to hear the voices of women from Black and minority ethnic groups.
In some areas where the population was mainly White, inspectors felt that services viewed engaging with women from minority groups as a low priority. Some services told us they had found it challenging to engage with their local population but had no clear strategies on how they would tackle this. In other services, most of the work that was being done was not targeted towards specific communities and, as a result, was not representative of women with higher risks of poor outcomes, such as women from Black and minority ethnic groups.
A number of services acknowledged that work to engage women from Black and minority ethnic groups was lacking, or staff were unable to articulate whether anything was being done.
However, positive examples of targeted engagement we heard of included:
- One service participating in a Local Maternity System survey around cultural safety in working with women from Black and minority ethnic groups.
- One service’s MVP working with the Local Maternity System to recruit diversity champions to build links with local communities.
- Another service, supported by their MVP, holding weekly focus groups to better understand the issues faced by women from Black, Asian and minority ethnic groups.
A number of MVP chairs we spoke with raised concerns over how their trusts communicated with women during the course of the pandemic. In particular, two chairs felt that the MVP social media pages had become the sole method of communicating updates to women using the maternity services (which lacked their own social media pages). One chair acknowledged how risky this was because not everyone was aware of, or used, the MVP’s Facebook page. Another MVP felt that the language their maternity service had used to communicate information around accessing maternity services during the pandemic was not reassuring to women.
Maternity Voices Partnerships and engagement
Key points
- We heard that working relationships between MVP chairs and maternity services varied. While some MVP chairs felt they had a strong working relationship, others felt unsupported by their service.
- MVP chairs told us that they were concerned MVPs were not fully representative of their local area, and that engagement with Black and minority ethnic women could be improved.
- MVP chairs told us that funding was a major challenge to effective engagement and enabling women from Black and minority ethnic groups or from deprived areas to get involved.
- We heard that reliance on digital technology during the pandemic made it harder for women without the access to, or skills to use, digital technology to keep informed and have their voices heard.
Joint working between trusts and Maternity Voices Partnerships
As part of our review, in seven services we looked directly at how well they were working with their local Maternity Voices Partnerships (MVP).
Several services we visited felt they had a good relationship with their MVP. Services also told us they had a range of interactions with MVPs and that the consultant midwife was often the key point of contact for the MVP. Two services described different meetings or workstreams that the MVP was involved in at the service, including the labour ward forum, weekly sitrep meetings and the maternity improvement group. Three services told us that they attended MVP meetings.
Most services were able to describe examples of where they had worked together with the MVP to engage their local community. This included working with the MVP to review communications and online content, sharing messages within the community, and supporting Q&A sessions on Facebook to collect feedback.
This was supported by our interviews with chairs of MVPs who told us that, at a minimum, they had worked with their local service to review outward-facing documents produced by the service to ensure they were accessible to women (for example, personal care plans, information around labour and COVID-19 information packs).
While these examples are positive, through our engagement with MVPs, Five X More and National Maternity Voices, we heard concerns that reliance on digital technology to engage women and provide them with the information they needed could exclude women who do not have the access to, or skills to use, digital technology.
In some cases, MVP chairs we spoke with felt they had a strong working relationship with the service. In these cases, we heard examples of greater co-working and collaboration, and that the MVP was embedded more deeply within the workings of the trust. One particular MVP chair described how they were invited to be part of a panel for an internal review looking at how the trust was meeting safety recommendations.
“I have been really involved in everything and co-producing as well, not just reviewing things as a tick-box exercise. We’re involved from the start with any big changes and our opinions are taken forward…[I’m] treated as an equal.” MVP chair
However, this was not the experience of all MVP chairs we spoke with, some of whom viewed their relationship with the maternity service more negatively. In these cases, the MVP chairs told us that they felt unsupported by the trust and that it was down to the MVP to lead the relationship.
We heard that negative relationships were also characterised by poor communication between the trust and the MVP. This included a lack of transparency around the governance processes and MVPs not kept updated and informed about relevant work, as well as a lack of response and follow up to feedback.
Embedding the role of the MVP into trust activities
Where the MVPs we spoke with felt that working with maternity services was not consistently collaborative, we heard that the role of the MVP was not well understood by the trust and was not strategically embedded within the trust’s processes.
“[It] feels shambolic, I think sometimes [the trust] are just not sure where [the MVP] could and should be because they are constantly responding to things rather than strategically thinking ‘it would be helpful to have the MVP here, here and here – let’s get those in the diary and start a conversation about complaints and safety.” MVP chair
This had led to issues such as the MVP not being involved early enough in the process to give meaningful feedback and the trust being defensive to suggestions from the MVP. For example, we heard how one MVP was sometimes only given sight of documents after they had already been shared with the public in what felt like a tick-box exercise rather than meaningful co-production.
Raising concerns over safety
The MVP chairs we spoke with generally had clear and direct channels of contact via phone or email with the head of midwifery or other specified roles at the maternity service. They also felt confident that they would be able to raise safety concerns.
However, some MVP chairs told us that they felt unsure as to how they would raise a safety concern with the service and were unaware of any official documented procedures around this. Some chairs told us that they had experienced a lack of transparency around the governance processes and lack of follow-up in response to safety concerns.
“When concerns arise, one thing that puts us in quite a compromised position is we hear some things that are really quite worrying and then we pass those worrying things up and if something doesn’t happen as a result of them… [it] devalues our status as MVP and that’s problematic because it can erode that trust that we work hard to build.” MVP chair
MVPs and engagement
MVP chairs we spoke with told us that they used a variety of methods to gather feedback from women who use maternity services. These including online listening events where people who use services could openly share their experiences, as well as focused surveys on topics such as reduced foetal movements.
Engagement with women from Black and minority ethnic groups or other minority groups was mostly through local groups that represented these communities. The MVP chairs we spoke with were at different stages of their journey in setting up these networks.
Most MVP chairs we spoke with felt that MVPs needed to improve how they engaged with women from minority groups, and ensure that they were better represented. There was little evidence that the maternity services proactively supported the MVPs we spoke with to engage specifically with women from Black or minority ethnic groups or other women who might be more likely to have poorer experience or outcomes from care.
“I don’t think the trust are actively saying ‘how are you reaching [ethnic minorities]?’ because they’ve got so much other stuff they are chasing their tails with.” MVP chair
One MVP chair told us that it is typically only mothers with fewer demands on their time and more financial freedom that were able to contribute their views to the MVP. They felt that greater incentives need to be available to support mothers who are having to juggle work, children and other responsibilities to share their feedback with the MVP.
This was corroborated through our engagement with Five X More and National Maternity Voices who also highlighted the disparity in funding between different MVPs. People we spoke with highlighted how pay for the MVP chair role varies across regions, and that chairs are increasingly expected to go above and beyond their paid role. They felt that this was neither reasonable nor sustainable without an increase in contracted hours. We also heard how these issues could be a barrier to women from some communities or groups getting involved, perpetuating issues with a lack of diversity.
Some chairs we spoke with felt that the lack of diversity among MVP members limited how well they could engage with other groups of women. Connecting with women who do not speak English as a first language was noted as a particular challenge, especially as most avenues of engagement (Facebook pages, WhatsApp groups, listening events, etc) are conducted in English.
A couple of MVPs had tried reaching out to women via religious organisations, such as mosques and synagogues, but did not find this approach productive. We heard that general appeals on social media to increase the representation of Black and minority ethnic groups within the MVP were also met with limited success. This contrasts with the national Black Maternity Survey led by Five X More, which had a good response.
A major barrier to engagement was the inability to meet face-to-face during the pandemic. Before this, events such as ‘walking the patch’ to talk to mothers on the ward and visiting children’s centres and baby groups presented opportunities to connect with women who may not have otherwise contacted the MVP.
We also heard that some women found online sessions intimidating as these could be attended by up to 30 professionals. The need to limit engagement to online platforms during the pandemic has widened inequalities for women who do not have the resources, know-how or confidence in using digital technology. In other words, digital exclusion has made it harder to hear the voices of women who are already at risk of not being heard.
That being said, the MVP chairs we spoke with did recognise that the use of digital technology had created some new opportunities for better engagement. One MVP noted that attendance of their meetings had increased, possibly because where women are less mobile with a newborn baby or lack transport they may find it easier to attend MVP meetings virtually. Online meetings have also facilitated the attendance of professionals from the maternity service as well as community group representatives and other professional stakeholders.
Next steps
For maternity services and local maternity systems
The key concerns identified in our report are not new. It is important that all maternity services, supported by wider system partners, embed changes quickly and effectively to address them. Achieving this will require a focus in the following areas:
- Leadership: In line with essential action 2 of the first Ockenden review, Boards must take effective ownership of the safety of maternity services. This includes ensuring that they have high quality, multidisciplinary leadership and positive learning cultures. They must seek assurance that staff feel free to raise concerns, that their concerns and adverse events lead to learning and improvement and that individual maternity staff competencies are assured.
- Voices and choices: In line with the Cumberlege review ‘First do no harm’, maternity services must ensure that all women and their families have information and support that allows them to make choices about their care. This includes listening to individual women and fully explaining choices, in an accessible way throughout the pregnancy journey. This includes, for example, working effectively with interpreters.
- Engagement: As supported by the findings of 'Better Births' and 'First do no harm', local maternity systems need to improve how they engage with, learn from and listen to the needs of women, particularly women from Black and minority ethnic groups. They also need to make sure that targeted engagement work is appropriately resourced.
- Data and risk: Services and systems should use ethnicity data they collect to review safety outcomes for women from Black and minority ethnic groups, and take action in response to risk factors. This includes working with Black and minority ethnic women to personalise care and reduce inequality of outcomes.
For CQC
In line with our strategic theme, safety through learning, we will continue to promote and check on open and honest cultures within maternity services. We will continue to:
- focus on the quality of maternity leadership teams, ensuring they understand the day-to-day running of the service, are listening to staff and ensuring they feel free to speak up, and that they foster a culture that drives continuous improvements in safety.
- look at how leadership teams ensure multidisciplinary staff who work together are training and learning together without barriers, and that staff are supported to develop and maintain individual core competencies and to work effectively as a team at all times.
- assess the transparency of services, ensuring that they embrace learning and reporting cultures and that there is accountability and trust.
Tackling health inequalities is a core ambition of our new strategy. As part of this we will:
- continue to ask maternity services about work on maternity equity and engagement during inspection and monitoring activity
- continue to learn from women who use services and who face inequality
- apply what we have learned to other core services and areas of our work
- consider equity and engagement as issues that impact on safety
- expect services to use people’s experiences and equality data to review and act on outcomes and respond to the needs of their local population
- continue to improve how we work with equality data to assess safety and quality of people’s care and work with others to do this.
Find out more
This print option will include all the text on this page, with every section expanded
Maternity focussed inspections - equity, engagement and teamwork: equality impact assessment