Bath and North East Somerset Council: local authority assessment
Downloads
Overall summary
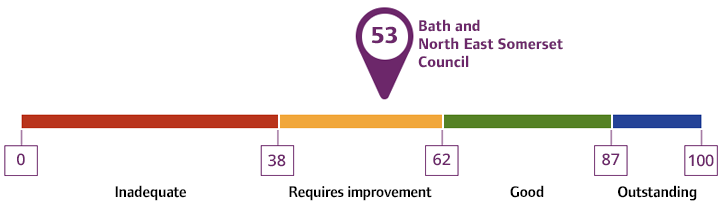
Local authority rating and score
Quality statement scores
Summary of people's experiences
People’s experiences of accessing adult social care in B&NES were mixed. Data to evidence whether people were able to access Care Act 2014 Assessments effectively via the first response team was limited. Staff told us people would contact the first response team and staff would ask questions in a strengths-based way to determine whether they required a Care Act assessment. If no assessment was required, staff would signpost and provide them with information about appropriate services in the community. Data provided for July 2024 showed only 2 people were referred to the teams for a Care Act assessment following contact with the first response team, data was not recorded for people who were signposted to other services. Most people who had accessed services told us they were able to do so easily. However, some people gave feedback that information was harder to find, especially if they were less familiar with digital platforms.
Feedback from people about the approach of staff was positive. People reported receiving assessments from kind, dedicated, and passionate staff who had a positive approach. Care Act assessments were completed in a strengths-based way, promoting independence and focusing on what people could do. Leaders told us they felt assessments were strengths based. However, leaders identified some improvements that were needed in support plans to ensure they were more creative, person centered and could flexibly meet people’s needs.
Approximately 60% of people needing services were self-funders (this meant they would be funding the full cost of their care). Staff understood the need to provide a Care Act assessment and offer those funding their own care support to find services. The local authority charged an administration fee to support this, or people paying the full cost of their care could access services independently.
The experience of unpaid carers was mixed. We heard how people found it difficult to access advice and information regarding what support the local authority could give them. Unpaid carers assessments were not always carried out in a timely manner, and carers told us they were unclear about who carried out carers assessments and what support the Carers Centre provided. The Carers Centre confirmed they did not carry out carers assessments for adult unpaid carers but did carry out carers assessments for young carers. Some unpaid carers were unsure what benefits a carers assessment would have and how this would help to support them and their loved ones. Leaders identified the need to improve the carers offer and were looking at ways of how to improve this. One action taken to improve carers support was via the carers co-production group. Feedback from carers regarding the co-production group was positive.
People worked in co-production with the local authority to get people's voice and views heard. People told us this work was positive, and they felt listened to and respected and were looking forward to seeing how their input had improved practice and accessibility for people who use services and their carers.
Staff worked with partners to meet people’s needs holistically. We received positive feedback about voluntary services and heard examples of voluntary sector services supporting people with minimal care and support needs to return home quickly and effectively from hospital. People received support from staff who worked in a collaborative way. Leaders identified the need to continue to improve and embed collaborative working within teams.
Summary of strengths, areas for development and next steps
This assessment took place during a time of ongoing transformation. The local authority had recently brought their Care Act 2014 functions in-house and many policies, processes and governance procedures were being reviewed and embedded. Following the transfer back in-house, adult social care was also reviewing job roles and team structures. In addition, the whole council was going through a transformation with the vision “Being Our Best” which was intended to ensure every contact with the local authority was the best and improved each person’s interaction with the local authority. Leaders and managers were also being introduced to an improved, more in-depth, version of their Power BI data system to support them with oversight and governance. The improved version had not yet been fully implemented at the time of our assessment however, leaders told us the original version was still being used by leaders and managers to support with oversight.
Feedback from staff regarding the technicalities of the transfer back in-house was positive. Staff told us the move went smoothly, and they felt well informed and prepared for the transfer. Staff told us the training offer has improved since moving back in house and that training was easily accessible, informative and relevant to their job roles. However, the overall council transformation, change in job profiles, and potential future structures of teams, were causing staff anxiety and staff did not feel the process was well communicated. Staff spoke positively about their managers and senior leaders and felt supported in supervision. However, staff told us they felt there needed to be more oversight and decision-making support in some teams.
Feedback from health partners was positive. We heard how health, adult social care, the HCRG group and the community and voluntary sector were working together in the Community Wellbeing Hub to prevent, reduce and delay people’s care needs. Leaders identified a need for more collaborative working so people would only have to tell their story once more promotion of people’s independence and to reduce the need for care and support. Health partners and leaders described positive working relationships and joint working to achieve shared aims. Health partners, leaders and staff understood the importance of the voluntary and community sector to meet their strategic aims around prevention. Feedback from the voluntary sector was positive. However, some organisations flagged issues around capacity and explained they had waiting lists due to the increase in referrals sent to them from the local authority.
National data showed the experiences of people living in B&NES were mainly positive or in line with national trends. Data showed people felt in control of their own lives and were satisfied with the care and support they received. National data showed the direct payment uptake was low.
Leaders had a good understanding of where they needed to improve. Where shortfalls were identified, plans were in place to address them though some plans and changes were yet to take place and embed. Changes had already been made to improve co-production, and leaders identified the need to continue to improve co-production and other ways to gain people's feedback on their experiences. The carers co- production was particularly positive, carers told us they felt listened to and respected. They were looking forward to seeing the changes and suggestions they made regarding the carer’s strategy being put into practice.
Unpaid carers feedback was mixed, carers did not always know what support and advice was available to them and what impact a carers assessment could have. Some carers told us they had been in a caring role for some time before being offered a carers assessment. The local authority has identified the need to improve the carers offer.
There were gaps in knowledge of some leaders regarding the understanding of their diverse communities and seldom heard groups. We heard how adult social care, and public health had worked together to reach the boating and traveller community and how the Director of Adult Social Services (DASS) represented the local authority in the lesbian, gay, bisexual, transgender or queer (LGBTQ+) community group.
Data collected by the local authority did not support the identification of people whose voices are seldom heard. For example, it was not compulsory to add a person’s religion or ethnicity to the recording system when creating a record at the front door, this meant there were potential inconsistencies in the monitoring of people from seldom heard groups and whether they had interacted with the local authority.
Waiting times for Care Act assessments and reviews varied from team to team. Some people waited longer than the adult social care targets set by the local authority. Staff told us staffing issues were having an impact on waiting lists for people awaiting an occupational therapy assessment, and the reviewing team had people who were waiting over a year for their annual review.
Leaders had positive and ambitious plans to improve adult social care in the future including improving performance, gaining people’s voice, working collaboratively and improving governance, oversight and use of data to inform changes and improvements to practice. Leaders identified the gaps in governance and understood the importance of embedding changes in order to improve practice.