London Borough of Ealing: local authority assessment
Downloads
Overall summary
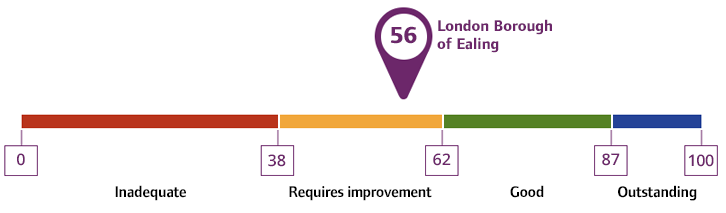
Local authority rating and score
Quality statement scores
Summary of people's experiences
People and their carers gave us mixed feedback of their experiences of local authority care and support services. Some people we spoke to said it was difficult to get in touch with the local authority. There were concerns about an overreliance on online information, and that the local authority’s website was difficult to navigate. People were more positive about the services they received, including commissioned services to meet their needs and reablement.
People’s experiences of accessing adult social care in Ealing was mixed. People were not always able to access information and advice, Care Act 2014 assessments, reviews and safeguarding support in a timely way. Some people described a positive assessment experience with knowledgeable and caring staff and that subsequent care, once in place, supported their preferences. Others told us there could be improvements in communication and the ways they were supported to access further services in the community.
People told us they waited for equipment and adaptations that supported them to remain independent at home. People were generally positive about their assessment and equipment once in place. Young people moving to adults’ services and people coming out of hospital were generally positive about their support. Some carers told us that they did not receive the longer-term support they needed to be able to effectively meet their needs. Carers told us there was some support available to them in the area, but that support could be difficult to access.
People often had choice of care providers, especially when considering homecare provision. People told us they received care and support that considered their cultural, ethnic, and religious needs.
Some people told us about how the local authority was including in them in strategy and decision making which supported them to raise concerns and support solutions. People told us they felt positive about this change.
Summary of strengths, areas for development and next steps
There were waiting lists for assessments in the borough, including Care Act assessments, reviews, and assessments for equipment or adaptations. Leaders told us there was rising demand and complexity of needs in the borough. Senior staff and managers regularly reviewed waiting lists to reprioritise allocations of work and used additional measures and resources to reduce waiting lists. These actions were making some improvements to people’s waiting times for assessments.
The local authority was clear about its responsibility to complete carers assessments. Staff understood the need to support carers. Carers could not always access services in their area that supported their wellbeing. Not all staff could articulate their role in identifying young carers who supported an adult with Care Act needs, though this was being addressed by the local authority in their developing Carers Strategy.
There were some effective partnership arrangements with external and internal partners in place in the borough, including for hospital discharge and transitions for young people. Most community and voluntary sector agencies we spoke to were pleased with the direction of travel in how the local authority was working with communities, including for example, the Community Connectors programme.
Where there were safeguarding concerns, immediate safety plans were in place. However, safeguarding enquiries were not always allocated promptly and there were waiting lists. When a safeguarding social worker was allocated, staff were knowledgeable, skilled and supportive. Some staff were concerned the safeguarding team received lots of contacts that were not related to safeguarding. This meant frontline staff could not be sure that all partners understood safeguarding or made safeguarding personal. Though some support was provided to partners at the time of our assessment, staff felt more support was needed for partners to understand safeguarding.
People in the local authority accessed a variety of care provision within and outside of the local authority area. Leaders told us they had identified gaps in services relating to specialist dementia provision, support for people expressing an emotional reaction or needs, complex nursing care, and supported living. The local authority had plans in place, including the introduction of new services to reduce these gaps.
There was a clear ambition to reduce inequality and improve people’s outcomes through quality services, throughout management and governance processes. Leaders had identified that people were not always receiving services that improved their experiences and outcomes, and they had taken action to address this, such as through improved monitoring. This work was ongoing at the time of our assessment. Clear governance was in place which had been strengthened by the inclusion of community advocacy and pressure groups in scrutinising the local authority’s work. People’s voice in governance arrangements was being considered through the ongoing development of the existing co-production groups. The local authority recognised that there was limited data analysis in place that supported their understanding of themes, trends, and people’s experiences. Leaders told us they were continuing to improve ways of gaining feedback from people, and how they used it to improve practice.
Governance and management arrangements were in place and these provided visibility and assurance on key priorities. There was line of sight on areas where people were not achieving good outcomes. Improvement actions were being developed or were in progress at the time of our assessment and we were given examples of where some of these had had a positive impact. The local authority used some of the information it had available to support strategic planning, however the local authority recognised more work was needed in developing its it in house performance and analytics function and had recently brought the resources inhouse from the corporate centre to support this.
People's experiences had begun to be represented on appropriate boards, such as the disability and long-term conditions board, by relevant partner organisations from the community. Work was underway to develop this approach.
Staff were proud of the work they did in the borough. Staff demonstrated a person-centred strength-based approach in assessing needs and developing care plans. They were knowledgeable about services in the community and could signpost people to services that would meet their needs. Staff we spoke with felt supported through supervision and reflective practice and by a visible and compassionate management and senior leadership team. Staff had opportunities to develop and complete training or required learning, though some staff indicated workload pressure did limit their ability to do this.
There was a positive culture of learning and innovation at the local authority. Staff felt able to share their ideas and concerns and they were listened to. The local authority had implemented assessment review and resource review panels to support improved practice and opportunities for learning. The local authority was trialling several examples of innovative technology and artificial intelligence to reduce the administrative burden on staff and increase the time they could spend with people.